 May is Mental Health Awareness Month. The VA Office of Health Equity is pleased to partner with VA’s Make the Connection campaign to raise awareness of mental health, effective treatments, and efforts to support those who face mental health challenges.
May is Mental Health Awareness Month. The VA Office of Health Equity is pleased to partner with VA’s Make the Connection campaign to raise awareness of mental health, effective treatments, and efforts to support those who face mental health challenges. VA’s Make the Connection campaign encourages Veterans, Servicemembers, and their families to connect with local sources of mental health support when they need them.
Here are some of other ways that the VA Office of Health Equity is supporting VA Secretary Dr. David J. Shulkin’s breakthrough in Veteran suicide prevention priorityby championing the reduction of mental health disparities especially among vulnerable Veterans: Apply an equity lens to Veteran suicide risk and mortality data to inform culturally appropriate and tailored prevention strategies for vulnerable Veteran populations on suicide prevention. Additional ways include:
- Data by sex, race/ethnicity & military era/period of service
- Cultural competency training that includes military culture
- Holistic approaches that incorporate social determinants of health
- Screening for changes in family & social support that trigger action
- Partnerships with cross section of vulnerable populations & stakeholders
- Culturally sensitive outreach & treatment connection options
- Use of peer support & community health workers
- Review and encourage outreach to Veterans who do not receive VA care
- Consider the impact of the intersection of disparities and social and neighborhood factors for vulnerable Veterans
- Health Disparities in Quality Indicators of Healthcare Among Adults with Mental Illness--2014
- Blosnich, J. R., Mays, V. M., Cochran, S. D. (2014). Suicidality Among Veterans: Implications of Sexual Minority Status. American Journal of Public Health, 104(S4): S535-S537.
- Blosnich, J. R., Gordon, A. J., Bossarte, R. M. (2014). Suicidal Ideation and Mental Distress Among Adults With Military Service History: Results from 5 US States, 2010. American Journal of Public Health, 104(S4): S595-S602.
- Brown, G. R., Jones, K. T. (2015). Mental Health and Medical Health Disparities in 5135 Transgender Veterans Receiving Healthcare in the Veterans Health Administration: A Case-Control Study. LGBT Health.
- Copeland, L. A., McIntyre, R. T., Stock, E. M., Zeber, J. E., MacCarthy, D. J., Pugh, M. J. (2014). Prevalence of Suicidality Among Hispanic and African American Veterans Following Surgery. American Journal of Public Health, 104(S4): S603-S608.
- OHE Champions Health Equity Issues for Veterans and You Can Get Involved

The VA Office of Health Equity had the pleasure of sharing information on Veteran health equity and several tools with VA Senior Leaders at a recent business meeting in Leesburg, Virginia. Below are just a few of the tools we shared:
- Veterans Journey with High Blood Pressure Videos for viewing in waiting rooms and common areas
- Virtual Patient Health Equity Training Modules as a training tool and to increase awareness of Veteran health equity issues
- National Veteran Health Equity Report for details of patterns and rates of health conditions for vulnerable Veteran groups
Here are ways that you can get involved
- Ask your medical provider or leadership team about reducing health disparities among Veterans and efforts they can implement to assist all Veterans in achieving their highest health and wellbeing.
- Learn more about efforts to reduce Veteran health disparities by downloading and sharing the VA Health Equity Action Plan.
- Visit the Office of Health Equity Tools Page to find trainings and learn more about things you can do to improve your health and the health others you care about.
Health Equity Day Video Keynote Link Update
 Dr. Uchenna S. Uchendu, VA OHE Chief Officer, delivered a video keynote at the inaugural VA Western New York Healthcare System’s Health Equity Day on Tuesday, April 25, 2017. Unfortunately, some may have experienced issues with the link to the video keynote that we previously shared. Fortunately, the new link to the video is available below.
Dr. Uchenna S. Uchendu, VA OHE Chief Officer, delivered a video keynote at the inaugural VA Western New York Healthcare System’s Health Equity Day on Tuesday, April 25, 2017. Unfortunately, some may have experienced issues with the link to the video keynote that we previously shared. Fortunately, the new link to the video is available below. Please watch the video, share your thoughts, and encourage your peers to do the same to learn more about VA Office of Health Equity and some of the way we are championing health equity for Veterans.
VIEW VIDEO KEYNOTE
Our sincerest apologies for any issues experienced.
U.S. Department of Veterans Affairs
810 Vermont Avenue, NorthWest
Washington D.C. 20420, United States
-------
BLS Data - April 2017 from VA Office of Economic Opportunity in Washington, D.C., United States for Friday, 5 May 2017
BLS Data - April 2017 from VA Office of Economic Opportunity in Washington, D.C., United States for Friday, 5 May 2017
Colleagues and Fellow Veterans,
As with the first Friday of each month, the BLS employment statistics were released today. Attached is our monthly ‘cheat sheet’ for your use and information. The national unemployment rate for April 2017 decreased slightly from 4.5% to 4.4% and the Veteran unemployment numbers for April 2017 decreased from 3.9% to 3.7%.
Thanks to all of you who are working directly or indirectly, to ensure our Veterans have meaningful employment.
BLS_Employment_Data_-_April_2017.pdf
V/R
Curtis L. Coy
Deputy Under Secretary for Economic Opportunity
Veterans Benefits Administration
U.S. Department of Veterans Affairs
Washington, D.C. 20420, United States
VA Core Values: Integrity, Commitment, Advocacy, Respect, Excellence (“I CARE”)
Please Remember:
If you would like to review prior messages sent through this listserv, click http://benefits.va.gov/vow/economic_opportunity.asp
If you would like to research, find, access, and, in time, manage your VA benefits and personal information please visit and/or register at https://www.ebenefits.va.gov/ebenefits-portal/ebenefits.portal.
As with the first Friday of each month, the BLS employment statistics were released today. Attached is our monthly ‘cheat sheet’ for your use and information. The national unemployment rate for April 2017 decreased slightly from 4.5% to 4.4% and the Veteran unemployment numbers for April 2017 decreased from 3.9% to 3.7%.
Thanks to all of you who are working directly or indirectly, to ensure our Veterans have meaningful employment.
BLS_Employment_Data_-_April_2017.pdf
V/R
Curtis L. Coy
Deputy Under Secretary for Economic Opportunity
Veterans Benefits Administration
U.S. Department of Veterans Affairs
Washington, D.C. 20420, United States
VA Core Values: Integrity, Commitment, Advocacy, Respect, Excellence (“I CARE”)
Please Remember:
If you would like to review prior messages sent through this listserv, click http://benefits.va.gov/vow/economic_opportunity.asp
If you would like to research, find, access, and, in time, manage your VA benefits and personal information please visit and/or register at https://www.ebenefits.va.gov/ebenefits-portal/ebenefits.portal.
-------
VAOIG - Administrative Summaries of Investigation Regarding Wait Times - Alabama, Arizona, District of Columbia, Georgia, Louisiana, Massachusetts, Nevada from Veterans Affairs Office of Inspector General (OIG) in Washington, D.C., United States for Friday, 5 May 2017

The Department of Veterans Affairs, Office of Inspector General (OIG), conducted extensive work related to allegations of wait time manipulation after the allegations at the Phoenix VA Health Care System in April 2014. Since that event and through fiscal year 2015, we have received numerous allegations related to wait time manipulation at VA facilities nationwide from veterans, VA employees, and Members of Congress that were investigated by OIG criminal investigators.
At this time, OIG has completed more than 100 criminal investigations related to wait times and provided information to VA’s Office of Accountability Review for appropriate action. It has always been our intention to release information regarding the findings of these investigations at a time when doing so would not impede any planned prosecutive or administrative action. As other administrative summaries of investigation are completed, we intend to post them to our website so that veterans and Congress have a complete picture of the work conducted in their state.
You may view and download these administrative summaries of investigation by clicking on the link to our webpage at www.va.gov/oig/publications/administrative-summaries-of-investigation.asp and selecting the appropriate state. The individual summaries may also be accessed by selecting the weblinks below.
VAOIG - Administrative Summaries of Investigation Regarding Wait Times - Alabama, Arizona, District of Columbia, Georgia, Louisiana, Massachusetts, Nevada from Veterans Affairs Office of Inspector General (OIG) in Washington, D.C., United States for Friday, 5 May 2017

The Department of Veterans Affairs, Office of Inspector General (OIG), conducted extensive work related to allegations of wait time manipulation after the allegations at the Phoenix VA Health Care System in April 2014. Since that event and through fiscal year 2015, we have received numerous allegations related to wait time manipulation at VA facilities nationwide from veterans, VA employees, and Members of Congress that were investigated by OIG criminal investigators.
At this time, OIG has completed more than 100 criminal investigations related to wait times and provided information to VA’s Office of Accountability Review for appropriate action. It has always been our intention to release information regarding the findings of these investigations at a time when doing so would not impede any planned prosecutive or administrative action. As other administrative summaries of investigation are completed, we intend to post them to our website so that veterans and Congress have a complete picture of the work conducted in their state.
You may view and download these administrative summaries of investigation by clicking on the link to our webpage at www.va.gov/oig/publications/administrative-summaries-of-investigation.asp and selecting the appropriate state. The individual summaries may also be accessed by selecting the weblinks below.
- VA OIG Administrative Summary of Investigation at the Alexandria, Louisiana VA Medical Center (14-02890-93)
- VA OIG Administrative Summary of Investigation at the Atlanta, Georgia VA Medical Center (14-02890-127)
- VA OIG Administrative Summary of Investigation at the Atlanta, Georgia Health Eligibility Center (14-03368-97)
- VA OIG Administrative Summary of Investigation at the Augusta, Georgia VA Medical Center (14-02890-129)
- VA OIG Administrative Summary of Investigation at the Las Vegas, Nevada VA Medical Center (14-02890-104)
- VA OIG Administrative Summary of Investigation at the Montgomery, Alabama VA Medical Center (14-02890-112)
- VA OIG Administrative Summary of Investigation at the Montgomery and Tuskegee, Alabama VA Medical Centers (14-02890-96)
- VA OIG Administrative Summary of Investigation at the Phoenix, Arizona VA Medical Center (14-02890-126)
- VA OIG Administrative Summary of Investigation at the Phoenix, Arizona VA Medical Center and Gilbert, Arizona Community Based Outpatient Clinic (14-02890-110)
- VA OIG Administrative Summary of Investigation at the Washington, DC VA Medical Center (14-02890-116)
- VA OIG Administrative Summary of Investigation at the West Roxbury, Massachusetts Community Based Outpatient Clinic (14-02890-409)
-------
Make a difference for Veterans during Mental Health Awareness Month; Veteran helping other Veterans out of addiction from U.S. Department of Veterans Affairs in Washington, D.C., United States for Friday, 5 May 2017


[ABOVE] Veterans to showcase fitness at National Veterans Golden Age Games

A Veteran’s son: Thank you VA for being kind, compassionate, professional.
"At every point of the way, as we waited or were speaking to someone, it was apparent that these workers deeply believed in their mission to honor and serve those that served our country."

Use Your Voice: Make a difference for Veterans during Mental Health Awareness Month
Every May, VA recognizes Mental Health Awareness Month as an opportunity to raise public awareness and reduce the inaccurate and often damaging stereotypes associated with mental health conditions.

Air Force Veteran helping other Veterans out of addiction
Willie Raulerson is paying forward what VA has given him. He’s now one of seven full-time peer support specialists at the Tucson VA, helping other Veterans find their way out of addiction. He’s been at it, nearly every day, for six years.
New on VAntage Point:
Connect with VA:




VETERAN OF THE WEEK
This week we honor is Army Vietnam War Veteran Roy F. Burmeister.
Roy served with the 1st Infantry Division during the Vietnam War and after returning home, joined the Army Reserves. Over the following years, he trained with the military police and field artillery.
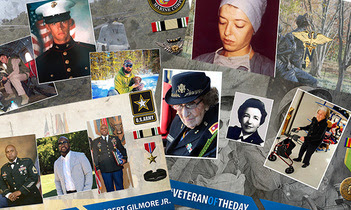
Nominate a special Veteran as #VeteranOfTheDay
It’s easy to nominate a Veteran. All it takes is an email to us with as much information as you can put together. Click on the picture to the left for an overview of how to put together a great #VeteranOfTheDay package.
Keep updated & let us know how we're doing.






Make a difference for Veterans during Mental Health Awareness Month; Veteran helping other Veterans out of addiction from U.S. Department of Veterans Affairs in Washington, D.C., United States for Friday, 5 May 2017


[ABOVE] Veterans to showcase fitness at National Veterans Golden Age Games

A Veteran’s son: Thank you VA for being kind, compassionate, professional.
"At every point of the way, as we waited or were speaking to someone, it was apparent that these workers deeply believed in their mission to honor and serve those that served our country."

Use Your Voice: Make a difference for Veterans during Mental Health Awareness Month
Every May, VA recognizes Mental Health Awareness Month as an opportunity to raise public awareness and reduce the inaccurate and often damaging stereotypes associated with mental health conditions.

Air Force Veteran helping other Veterans out of addiction
Willie Raulerson is paying forward what VA has given him. He’s now one of seven full-time peer support specialists at the Tucson VA, helping other Veterans find their way out of addiction. He’s been at it, nearly every day, for six years.
New on VAntage Point:
- VA partners with Department of Energy on big-data initiative to improve health care for Veterans
- VA and TAPS working together to support the families of America’s fallen heroes
- Using VA’s Million Veteran Program to identify genetic risk factors for alcohol, tobacco, and opioid use
- A look at some of the VA programs MST survivors chose to help them recover
- VA Innovators Network Accelerator is all about new ideas that give Veterans a reason to choose VA
- Retired Air Force officer, Vietnam Veteran heads to National Veterans Golden Age Games
- VA recognizes Mental Health Awareness Month with promotion of ‘Use Your Voice’ awareness program to urge Veterans to speak up about mental illness
- Head First: How the GE/NFL head health initiative became a catalyst for technology and innovation for brain trauma
- Faced with a choice to complain or take action, one group hit the road to serve Veterans
- Oregon Department of Veterans Affairs spearheads campaign to draw attention to women Veterans
- VA’s National Center for PTSD: In the vanguard of trauma research
- VA center in Texas to lead research into the top two signature wounds from wars in Afghanistan, the Middle East
- VA leader’s visit New Mexico’s Taos Pueblo Tribe focuses on improving access to Veteran health care
Connect with VA:
- Facebook - Veterans of the Day, Top VA news & videos
- Twitter - Veteran news from around the country
- Subscribe - Never miss a VA update
- Instagram - Top Veteran pictures from around the country
- Subscribe - This Week at VA podcast




VETERAN OF THE WEEK
This week we honor is Army Vietnam War Veteran Roy F. Burmeister.
Roy served with the 1st Infantry Division during the Vietnam War and after returning home, joined the Army Reserves. Over the following years, he trained with the military police and field artillery.
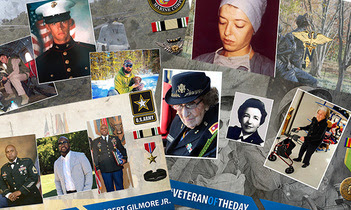
Nominate a special Veteran as #VeteranOfTheDay
It’s easy to nominate a Veteran. All it takes is an email to us with as much information as you can put together. Click on the picture to the left for an overview of how to put together a great #VeteranOfTheDay package.
Keep updated & let us know how we're doing.






-------
VAOIG - Administrative Investigation Advisory - Alleged Gross Mismanagement, Department of Veterans Affairs from Veterans Affairs Office of Inspector General (OIG) in Washington, D.C., United States for Friday, 5 May 2017

The Department of Veterans Affairs, Office of Inspector General (OIG) independently reviews allegations and conducts administrative investigations generally concerning high-ranking senior officials and other high profile matters of interest to Congress and the Department. While these reviews and investigations may result in the issuance of a formal report, they can also lead to the issuance of an administrative advisory to VA senior leadership. Advisories have been issued instead of reports if allegations are substantiated but no recommendations are made or are unsubstantiated during the course of the investigation and there is a need to notify VA leadership of the investigative results.
OIG’s intention is to maintain transparency with veterans, Congress, and the public by releasing information related to administrative investigative work completed by OIG. As other administrative investigation advisories are completed, they will be available on our website if they are not prohibited from public disclosure.
You may view and download these administrative investigation advisories by clicking on the link to our webpage at https://www.va.gov/oig/publications/administrative-investigation-advisories.asp. The individual advisory may also be accessed by selecting the weblink below.
-------
Military nurses develop diverse skills, capabilities from Military Health System in Washington, D.C., United States for Friday, 5 May 2017


Military nurses develop diverse skills, capabilities
Air Force Col. Erwin Gines was a young officer and emergency department nurse at what’s now the Wilford Hall Ambulatory Surgical Center in San Antonio when he volunteered to serve with a special operations critical care evacuation team. He deployed with the team serving Joint Task Force Viking during the initial invasion of Iraq in 2003. It was the only medical unit, and Gines was the only emergency critical care nurse.
Patient care, Gines quickly found out, was not his only duty. Military nurses develop diverse skills, capabilities
VAOIG - Administrative Investigation Advisory - Alleged Gross Mismanagement, Department of Veterans Affairs from Veterans Affairs Office of Inspector General (OIG) in Washington, D.C., United States for Friday, 5 May 2017

The Department of Veterans Affairs, Office of Inspector General (OIG) independently reviews allegations and conducts administrative investigations generally concerning high-ranking senior officials and other high profile matters of interest to Congress and the Department. While these reviews and investigations may result in the issuance of a formal report, they can also lead to the issuance of an administrative advisory to VA senior leadership. Advisories have been issued instead of reports if allegations are substantiated but no recommendations are made or are unsubstantiated during the course of the investigation and there is a need to notify VA leadership of the investigative results.
OIG’s intention is to maintain transparency with veterans, Congress, and the public by releasing information related to administrative investigative work completed by OIG. As other administrative investigation advisories are completed, they will be available on our website if they are not prohibited from public disclosure.
You may view and download these administrative investigation advisories by clicking on the link to our webpage at https://www.va.gov/oig/publications/administrative-investigation-advisories.asp. The individual advisory may also be accessed by selecting the weblink below.
-------
Military nurses develop diverse skills, capabilities from Military Health System in Washington, D.C., United States for Friday, 5 May 2017


Military nurses develop diverse skills, capabilities
Air Force Col. Erwin Gines was a young officer and emergency department nurse at what’s now the Wilford Hall Ambulatory Surgical Center in San Antonio when he volunteered to serve with a special operations critical care evacuation team. He deployed with the team serving Joint Task Force Viking during the initial invasion of Iraq in 2003. It was the only medical unit, and Gines was the only emergency critical care nurse.
Patient care, Gines quickly found out, was not his only duty. Military nurses develop diverse skills, capabilities
 Karyn Miller in 1976 at the beginning of a Navy nursing career that would take her from the Carolinas to Iceland and Guam. (Courtesy photo) by: Military Health System Communications Office
Karyn Miller in 1976 at the beginning of a Navy nursing career that would take her from the Carolinas to Iceland and Guam. (Courtesy photo) by: Military Health System Communications OfficeAir Force Col. Erwin Gines was a young officer and emergency department nurse at what’s now the Wilford Hall Ambulatory Surgical Center in San Antonio when he volunteered to serve with a special operations critical care evacuation team. He deployed with the team serving Joint Task Force Viking during the initial invasion of Iraq in 2003. It was the only medical unit, and Gines was the only emergency critical care nurse.
Patient care, Gines quickly found out, was not his only duty.
“We converted bare-bones rooms in old Iraqi administrative buildings into makeshift operating rooms, surgical suites, and critical care areas,” said Gines, now the 60th Inpatient Squadron commander at David Grant USAF Medical Center at Travis Air Force Base, California. “We did whatever we were asked to do.”
Nurses became a permanent part of the armed forces more than 100 years ago, and, like Gines, have shown initiative, flexibility, and commitment in both traditional and atypical roles. Read more about the history of military nursing part 1 and part 2.
Retired Army Col. Donna Wright was a junior officer and critical care nurse at Irwin Community Hospital in Fort Riley, Kansas, in 1971 when she was sent on a one-year tour of duty at 3rd Field Hospital in Saigon. The fixed facility treated wounded, injured, and ill service members brought from other locations in Vietnam.
For America, the Vietnam War was winding down, and Wright didn’t go out on patient transport calls. Still, she had challenges in her assignment in the critical care/post op recovery unit. She took care of a steady stream of patients, sometimes having to scramble to improvise because of shortages in basic medical supplies.
As Wright’s tour was ending, the hospital chaplain gave her an unusual assignment: Take a baby home with her to San Francisco, where the little girl’s adoptive parents were waiting. The baby sat on Wright’s lap during the long flight back to the United States.
Post-Vietnam, Wright’s assignments included directing critical-care training programs, first at Fitzsimons Army Medical Center in Aurora, Colorado, and then at what’s now the Walter Reed National Military Medical Center in Bethesda, Maryland. She said she found it rewarding to help the next generation of nurses develop skills and confidence.
“I was delighted to see how opportunities for nurses expanded during my career,” she said.
Retired Navy Lt. Cmdr. Karyn Miller had a nursing diploma and three years of work experience in a civilian hospital in her native Rhode Island when she joined the Navy in 1976. She earned a bachelor’s degree and also a master’s degree in human resources while she was in uniform.
After patient-care assignments in Iceland, North Carolina, and South Carolina, among other places, Miller was sent to Naval Base Guam. There, she implemented the first medical informatics system for the main base hospital and two large clinics. The system collected, analyzed, and presented data digitally and was the foundation for electronic health records.
“It was one of my biggest accomplishments,” Miller said, “and the hardest.”
Retired Navy Rear Adm. Betsy Morris served for more than 30 years in active duty and reserve assignments. “There were so many opportunities for professional growth and challenging assignments,” she said. Her duties included serving as a medical mobilization coordinator during Operation Desert Shield and Desert Storm in the early 1990s.
“Our job was to identify who among the 10,000-plus reserve medical personnel would help meet the mobilization requirements,” said Morris, a pediatric nurse practitioner in Virginia.
Morris, who graduated from the University of Delaware, decided to become a Navy nurse after recruiters came to campus her junior year.
Air Force 1st Lt. Kelly Dering, a medical surgical nurse at Travis, hasn’t been in uniform long enough to experience a nontraditional nurse assignment. But like those who have served before her, she’ll gladly answer the call of duty.
“I’ll be happy anywhere,” she said. “Bloom where you’re planted – that’s my mentality.”
Read More ...
Marine learns to seek help for his mental health, encourages other to do same
For years, Marine Gunnery Sgt. Mathew Barr tried to deny the damage done to his mental health during the Battle of Fallujah, Iraq, in 2004. But with help from the Military Health System, he was able to face his demons and get the treatment he needed.
“It was a grueling and gruesome fight,” said Barr. “When I got back home from my deployment, that’s when I couldn’t control my emotions and was angry all the time.”Marine learns to seek help for his mental health, encourages others to do same
 Marine Gunnery Sgt. Mathew Barr survived the Battle of Fallujah, Iraq, in 2004. But he then faced a new battle for his mental wellness. (Courtesy photo)
Marine Gunnery Sgt. Mathew Barr survived the Battle of Fallujah, Iraq, in 2004. But he then faced a new battle for his mental wellness. (Courtesy photo)Military Health System Communications Office
For years, Marine Gunnery Sgt. Mathew Barr tried to deny the damage done to his mental health during the Battle of Fallujah, Iraq, in 2004. But with help from the Military Health System, he was able to face his demons and get the treatment he needed.
“It was a grueling and gruesome fight,” said Barr. “When I got back home from my deployment, that’s when I couldn’t control my emotions and was angry all the time.”
As one of the most storied battles of recent Marine Corps history, the Battle of Fallujah took the lives of more than two dozen Marines and injured many more. Not all of those injuries were immediately apparent. A year later, Barr would return to Iraq, this time losing his commanding officer, a man Barr was responsible for protecting. The mental anguish was almost too much. “My job was to die for him, so I failed. I had a lot of regret and survivor’s guilt.”
 As one of the most storied battles of recent Marine Corps history, the Battle of Fallujah took the lives of more than two dozen Marines and injured many more. Not all of those injuries were immediately apparent. (Courtesy photo)
As one of the most storied battles of recent Marine Corps history, the Battle of Fallujah took the lives of more than two dozen Marines and injured many more. Not all of those injuries were immediately apparent. (Courtesy photo)Through years of denial and searching for the right treatment, Barr finally got the professional medical help he needed to heal his mental health at Marine Corps Base Quantico, Virginia, in 2013.
“I was diagnosed with a traumatic brain injury and post-traumatic stress disorder,” said Barr, acknowledging that he was caught up in the mindset that warriors don’t admit their injuries. “We can’t show weakness, because that could be exploited even within our own ranks. There’s a stigma.”
But Barr knew keeping himself mentally well is just as important as keeping his service rifle working properly. Plus, he knew he had to get help for the sake of his wife and two young children.
“I knew who he was,” said Callie Barr, Mathew’s high school sweetheart she married 13 years ago. When she reached a point after one argument where she considered walking out, he broke down, crying and admitted he has demons. “That’s what I needed to hear,” she said, “and we worked through his issues together.”
“I want to be a good father, good husband, and a good Marine,” he said. “I needed to do something about it, so I just did it.”
At Quantico, Barr connected with the therapy at a traumatic brain injury clinic, where he got treatment for the brain injuries he suffered years earlier, as well as help with his post-traumatic stress disorder. Some of his therapies there included art and music therapies, as well as water therapy that he said helped calm him and become more self-aware of his body and emotions. Not all therapies are available for service members at every clinic. Barr was also able to talk with counselors and chaplains who helped him work through his emotional issues. “It was pretty incredible, and I was really fortunate I got to do that,” said Barr.
“Going to a provider earlier, even if you’re trying to work things out yourself, can help, even with that self-care,” said Public Health Service Lt. Evette Pinder, a psychological epidemiologist at the Deployment Health Clinical Center, a part of the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury. “If a service member, battle buddy, line leader, or family member sees a person is struggling mentally, engage a provider at that point to get help solving problems and coping. The service member and everyone around them play a role.”
Not only did Barr seek help for himself through his health care provider, but now he’s encouraging other service members to do the same. He’s the latest profile in the Real Warriors Campaign, a multimedia public education effort designed to encourage help-seeking behavior among service members, veterans, and military families coping with invisible wounds. The campaign is key to the Defense Department’s overall effort to connect warriors and their families with appropriate care and support for psychological health concerns, supplementing what the services and Military Health System offer and trying to remove the stigma of seeking help.
“We think service members, such as Gunnery Sgt. Barr, telling their stories will help,” said Pinder. She said those who have returned from the battlefield with the invisible wounds of war don’t have to feel they are alone. There are resources.
Barr said people shouldn’t wait to use those resources.
“Reaching out for help is not a sign of weakness; it’s actually a sign of strength,” said Barr. “You need to be there 100 percent, not just to do your job in the military but to be there for your family.”
Read More ...




 Questions for MHS?
Questions for MHS? Contact Us
STAY CONNECTED:





-------
Healthcare Inspection – Consult Management Concerns, VA Greater Los Angeles Healthcare System, Los Angeles, California from Veterans Affairs Office of Inspector General (OIG) in Washington, D.C., United States for Thursday, 4 May 2017
Healthcare Inspection – Consult Management Concerns, VA Greater Los Angeles Healthcare System, Los Angeles, California
OIG conducted an inspection at the request of former Chairman Jeff Miller, Committee on Veterans' Affairs, US House of Representatives, to determine the validity of the allegation that 74 deceased patients had open consults at the VA Greater Los Angeles Healthcare System (facility), Los Angeles, CA. We identified 225 deceased patients who had 371 open or pending consults at the time of their deaths or had discontinued consults after their deaths. Of the 225 patients, we found 117 patients with 158 consults who experienced delays in obtaining requested consults. We substantiated that 43 percent (158/371) of consults were not timely because providers and scheduling staff did not consistently follow consult policy or procedures. We did not substantiate the allegation that patients experienced serious or severe impact with long-term consequences or organ dysfunctions or that patients died as a result of delayed consults. However, we identified two patients who experienced minor or intermediate clinical impacts. We found that providers entered incorrect inpatient/outpatient setting and/or urgency for 14 percent (52/371) of the reviewed consults. While not an allegation, we observed deficiencies in consult management practices contributing to the delays. Of the 158 delayed consults, we noted that facility staff did not: (a) timely act on clinical consult requests, (b) close completed consults or discontinue duplicate requests or consults no longer indicated, or (c) monitor the electronic wait list for Homemaker/Home Health Aide services. We recommended that the Facility Director ensure that providers assign the proper consult setting and urgency, staff take action within 7 days of a consult request or sooner if clinically indicated, staff timely close or discontinue consults, staff review the quality and timeliness of the cardiology care for one of the two patients who experienced intermediate clinical impact and take action if appropriate, and staff monitor and address the care needs of patients on the Homemaker/Home Health Aide services electronic wait list.-------
Healthcare Inspection – Consult Management Concerns, VA Greater Los Angeles Healthcare System, Los Angeles, California from Veterans Affairs Office of Inspector General (OIG) in Washington, D.C., United States for Thursday, 4 May 2017

Healthcare Inspection – Consult Management Concerns, VA Greater Los Angeles Healthcare System, Los Angeles, California
OIG conducted an inspection at the request of former Chairman Jeff Miller, Committee on Veterans' Affairs, US House of Representatives, to determine the validity of the allegation that 74 deceased patients had open consults at the VA Greater Los Angeles Healthcare System (facility), Los Angeles, CA. We identified 225 deceased patients who had 371 open or pending consults at the time of their deaths or had discontinued consults after their deaths. Of the 225 patients, we found 117 patients with 158 consults who experienced delays in obtaining requested consults. We substantiated that 43 percent (158/371) of consults were not timely because providers and scheduling staff did not consistently follow consult policy or procedures. We did not substantiate the allegation that patients experienced serious or severe impact with long-term consequences or organ dysfunctions or that patients died as a result of delayed consults. However, we identified two patients who experienced minor or intermediate clinical impacts. We found that providers entered incorrect inpatient/outpatient setting and/or urgency for 14 percent (52/371) of the reviewed consults. While not an allegation, we observed deficiencies in consult management practices contributing to the delays. Of the 158 delayed consults, we noted that facility staff did not: (a) timely act on clinical consult requests, (b) close completed consults or discontinue duplicate requests or consults no longer indicated, or (c) monitor the electronic wait list for Homemaker/Home Health Aide services. We recommended that the Facility Director ensure that providers assign the proper consult setting and urgency, staff take action within 7 days of a consult request or sooner if clinically indicated, staff timely close or discontinue consults, staff review the quality and timeliness of the cardiology care for one of the two patients who experienced intermediate clinical impact and take action if appropriate, and staff monitor and address the care needs of patients on the Homemaker/Home Health Aide services electronic wait list.-------
Veterans Health Administration
Office of Health Equity
810 Vermont Avenue, NorthWest
Washington, D.C. 20420, United States
-------
-------


No comments:
Post a Comment